DAP notes are a structured way to document therapy sessions, ensuring clarity and consistency. They consist of three sections:
- Data: Objective observations like client behavior, symptoms, and quotes.
- Assessment: Professional analysis of progress, challenges, and trends.
- Plan: Next steps, including interventions, assignments, and scheduling.
Why Use DAP Notes?
- Track client progress effectively.
- Maintain HIPAA-compliant records.
- Support continuity of care.
Who Uses Them?
Therapists, counselors, psychologists, and behavioral health specialists across various settings.
To write DAP notes:
- Stick to facts in the Data section.
- Provide clinical insights in the Assessment.
- Outline actionable steps in the Plan.
Tools like AI-powered platforms simplify the process, saving time while ensuring accuracy and compliance.
Understanding the DAP Format
The DAP format organizes therapy session documentation into three key sections. Each part plays a role in creating clear and effective clinical records that support client care.
The Data Section
The Data section focuses on objective details, avoiding personal interpretations [5].
Here’s what to include:
- Specific symptoms, behaviors, and important life events
- Observations of mental status
- Client’s response to past interventions
- Direct quotes or statements from the client
For instance, instead of writing “Client seemed anxious”, note specific details like, “Client exhibited rapid speech, fidgeting, and reported experiencing heart palpitations three times this week.”
The Assessment Section
This section connects observations to therapy goals and diagnoses [3]. It turns the collected data into meaningful clinical insights.
Include the following in the Assessment:
- Analysis of symptoms and behavior trends
- Progress toward therapy goals or diagnoses
- New challenges or concerns
- Changes in the client’s condition
- Professional impressions based on the session
The Plan Section
The Plan section outlines actionable steps based on the assessment [3][4].
A solid Plan should cover:
- Planned interventions and client assignments
- Adjustments to treatment approaches
- Scheduling of upcoming sessions
- Referrals or coordination with other professionals
Each DAP section should be distinct yet connected, ensuring thorough and useful documentation. Understanding the purpose of each section makes it easier to create effective notes.
Steps to Write DAP Notes
Creating effective DAP notes involves a structured method that ensures thorough yet efficient documentation. Here’s how to write clear and professional notes that meet clinical and legal standards.
Write Clearly and Concisely
Focus on clarity by sticking to observable facts and avoiding subjective language. Document specific behaviors and use direct quotes when they provide meaningful context.
Tips for clear documentation:
- Replace subjective language with observable facts.
- Record specific behaviors and responses.
- Use direct quotes only when they add relevant clinical insight.
- Avoid using clinical jargon unless absolutely necessary.
For example, instead of writing, “Client was very upset”, you could note, “Client tearfully stated, ‘I can’t handle the pressure anymore,’ while raising their voice.”
Maintain a Consistent Format
Every DAP note should follow a consistent structure that includes three key components: Data (objective facts and client statements), Assessment (clinical analysis and progress), and Plan (next steps). A standardized format keeps records organized and easy to reference, improving continuity of care.
Cover All Key Details
Each section of the DAP note should be thorough and include essential information:
- Data: Record symptoms, mental state, and relevant events.
- Assessment: Provide clinical impressions, analyze progress, and identify patterns.
- Plan: Outline interventions, assignments, and follow-up actions.
Be sure to document safety concerns, crisis interventions, or any major changes in the treatment approach. Comprehensive notes not only aid clinical decision-making but also ensure compliance with ethical and legal guidelines [4].
sbb-itb-8e8938b
Using AI Tools for DAP Notes
AI-powered tools are changing how mental health professionals handle documentation, making it easier to create DAP notes while sticking to clinical standards.
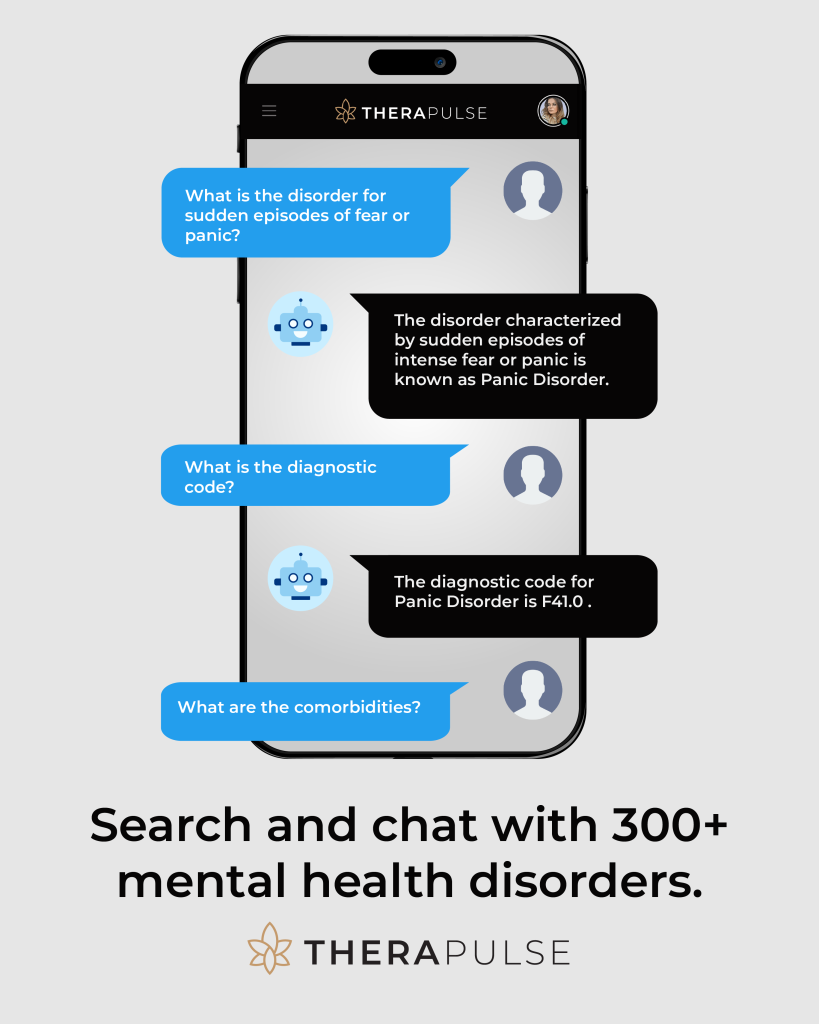
AI Solutions for DAP Notes
AI tools simplify the process of writing DAP notes by offering features like automated transcription to record verbal interactions, ready-to-use templates, integration with electronic health records (EHR), and secure, HIPAA-compliant data management. These tools fit seamlessly into existing workflows, freeing therapists to spend more time focusing on their clients.
Why Use AI Tools?
AI technology brings several benefits to DAP note creation, including:
- Automating repetitive tasks, saving time
- Keeping formatting consistent across records
- Ensuring data security and HIPAA compliance
- Accurately recording session details
- Organizing information to assist clinical decisions
How Therapulse Can Help
Therapulse is a great example of how AI is improving clinical documentation. It offers flexible pricing options to meet the needs of different practices. Plans start at $29/month for basic features and go up to $149/month for more advanced tools.
To get the most out of AI documentation tools, therapists should:
- Double-check the automated content for accuracy
- Adjust templates to fit their therapeutic methods
- Make sure all data handling complies with HIPAA rules
Conclusion
The Importance of DAP Notes
DAP notes play a crucial role in monitoring client progress and delivering consistent care. They go beyond being just clinical records – they shape treatment plans and aid in long-term strategies [4]. By following the DAP format, therapists can spot behavioral trends, document progress, and uphold professional standards, which all contribute to more effective client care [1][2].
Streamlining Documentation with Modern Tools
Given their importance, leveraging modern tools can make creating DAP notes more efficient while maintaining quality. AI-powered platforms, for instance, simplify the process and cut down on administrative work. Tools like Therapulse provide cost-effective solutions that adapt to practices of any size, making documentation easier to manage.
To get the most out of DAP notes in your practice:
- Stick to a standardized format for consistency
- Utilize AI tools to save time and ensure compliance
- Keep notes updated regularly for seamless care continuity
FAQs
Here are answers to some common questions therapists have about DAP notes and their documentation tools:
What is a DAP template?
A DAP template is a structured format for organizing therapy notes into three sections: Data, Assessment, and Plan. It ensures notes are clear and consistent across sessions while saving time and making records easier to access.
Can therapists use AI to write notes?
Yes, AI tools can assist therapists by simplifying the note-taking process. These tools can transcribe session audio into detailed therapy notes, reducing the need for manual writing while maintaining accuracy.
What is the difference between DAP and BIRP notes?
The main difference lies in how the information is structured and organized:
| Aspect | DAP Notes | BIRP Notes |
|---|---|---|
| Data Organization | Combines subjective and objective details in the Assessment section | Places all data under the Behavior section |
| Structure | Three sections: Data, Assessment, Plan | Four sections: Behavior, Intervention, Response, Plan |
| Focus | Broad assessment of the session | Focuses on specific behavioral details |
How to write DAP notes for therapy?
To write effective DAP notes, include the following:
- Objective observations: Document the client’s appearance and behavior.
- Subjective information: Note what the client shares about their thoughts and feelings.
- Clinical data: Record how the client responds to interventions during the session.
These FAQs cover common concerns, but using tools like AI can make your documentation process faster and more efficient without compromising quality.